Human – Digestive, Circulatory, Respiratory, Excretory, and Reproductive Systems
Introduction
The human body is a complex system of interconnected organs that perform essential physiological functions to sustain life. The digestive, circulatory, respiratory, excretory, and reproductive systems work in coordination to provide energy, oxygen, waste elimination, and reproduction. Understanding these systems is crucial for medical science, public health, and competitive exams like KPSC.
1. Digestive System
Key Functions
- Breakdown of food into simpler molecules.
- Absorption of nutrients into the bloodstream.
- Elimination of undigested waste.
Major Organs & Their Functions
- Mouth: Mechanical and enzymatic breakdown of food (saliva contains amylase).
- Esophagus: Peristalsis pushes food to the stomach.
- Stomach: Secretes gastric juices (HCl, pepsin) for protein digestion.
- Small Intestine: Absorbs nutrients via villi and microvilli.
- Liver: Produces bile for fat digestion.
- Pancreas: Secretes digestive enzymes and regulates blood sugar.
- Large Intestine: Absorbs water and forms feces.
- Anus: Expels waste materials.
Disorders
- Gastritis: Inflammation of the stomach lining.
- Gastroesophageal Reflux Disease (GERD): Acid reflux causing heartburn.
- Irritable Bowel Syndrome (IBS): Affects large intestine movement.
Relevant Government Schemes & Initiatives
- Poshan Abhiyaan: Addresses malnutrition.
- Mid-Day Meal Scheme: Provides nutritional food to school children.
2. Circulatory System
Key Functions
- Transport of oxygen, nutrients, hormones, and waste.
- Regulation of body temperature.
- Immunity through white blood cells.
Major Components
- Heart: Pumps blood (4 chambers—right/left atrium & ventricle).
- Blood Vessels: Arteries (carry oxygenated blood), veins (carry deoxygenated blood), capillaries (exchange of substances).
- Blood:
- Red Blood Cells (RBCs): Carry oxygen (hemoglobin).
- White Blood Cells (WBCs): Immunity.
- Platelets: Clotting.
Circulatory Disorders
- Hypertension: High blood pressure.
- Atherosclerosis: Plaque buildup in arteries.
- Anemia: Low RBC count.
Government Schemes & Initiatives
- Ayushman Bharat: Provides health coverage.
- National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases and Stroke (NPCDCS).
3. Respiratory System
Key Functions
- Oxygen intake and carbon dioxide expulsion.
- Cellular respiration for energy production.
- Regulation of blood pH.
Major Organs & Their Functions
- Nose & Nasal Cavity: Filters and moistens air.
- Trachea (Windpipe): Transports air to lungs.
- Bronchi & Bronchioles: Branch into lungs.
- Lungs: Gas exchange in alveoli (tiny air sacs).
- Diaphragm: Assists in breathing.
Respiratory Disorders
- Asthma: Narrowing of airways.
- Chronic Obstructive Pulmonary Disease (COPD): Progressive lung disease.
- Tuberculosis (TB): Bacterial lung infection.
Government Schemes & Initiatives
- National Tuberculosis Elimination Programme (NTEP).
- Clean Air Initiative: Addresses air pollution-related respiratory diseases.
4. Excretory System
Key Functions
- Removal of metabolic waste.
- Regulation of water and salt balance.
- Maintenance of blood pH.
Major Organs & Their Functions
- Kidneys: Filter blood, remove urea (nephrons as functional units).
- Ureters: Transport urine from kidneys to bladder.
- Urinary Bladder: Stores urine.
- Urethra: Excretes urine.
Excretory Disorders
- Kidney Stones: Hard deposits in kidneys.
- Urinary Tract Infections (UTI): Bacterial infection.
- Chronic Kidney Disease (CKD): Gradual kidney failure.
Government Schemes & Initiatives
- Pradhan Mantri National Dialysis Programme (PMNDP).
- Swachh Bharat Abhiyan: Promotes sanitation to prevent infections.
5. Reproductive System
Key Functions
- Production of gametes (sperm & ova).
- Fertilization and development of the fetus.
- Hormonal regulation of secondary sexual characteristics.
Male Reproductive System
- Testes: Produce sperm and testosterone.
- Vas Deferens: Transports sperm.
- Prostate & Seminal Vesicles: Produce seminal fluid.
- Penis: Transfers sperm.
Female Reproductive System
- Ovaries: Produce eggs and estrogen/progesterone.
- Fallopian Tubes: Site of fertilization.
- Uterus: Supports fetal development.
- Vagina: Birth canal.
Reproductive Disorders
- Polycystic Ovary Syndrome (PCOS): Hormonal imbalance in females.
- Infertility: Difficulty in conceiving.
- Prostate Cancer: Affects male reproductive health.
Government Schemes & Initiatives
- Rashtriya Kishor Swasthya Karyakram (RKSK): Adolescent reproductive health.
- Janani Suraksha Yojana (JSY): Safe motherhood initiative.
Committees & Reports
- National Health Policy (2017): Emphasizes universal health coverage.
- Kasturirangan Committee: Environmental impact on health.
- National Family Health Survey (NFHS): Provides reproductive health statistics.
Current Affairs & Relevance
- Covid-19 Impact: Respiratory system vulnerabilities.
- Artificial Organs: Advances in circulatory and excretory system treatments.
- Genetic Engineering in Reproduction: CRISPR technology applications.
Conclusion & Way Forward
The human body’s organ systems play a fundamental role in maintaining homeostasis. Advancements in medical research, biotechnology, and healthcare policies contribute significantly to addressing disorders related to these systems. Strengthening public health infrastructure, promoting awareness, and enhancing healthcare accessibility remain crucial for a healthier society.
Way Forward:
- Increased investment in biomedical research.
- Strengthening primary healthcare services.
- Enhanced public awareness on lifestyle diseases.
- Encouragement of organ donation and transplants.
Allopathic, Indian System of Medicine, Naturopathy, and Yoga (AYUSH)
Introduction
Healthcare in India encompasses multiple medical systems, including Allopathy, Ayurveda, Yoga, Naturopathy, Unani, Siddha, and Homeopathy (AYUSH). While Allopathy is the dominant medical system worldwide, traditional systems under AYUSH offer holistic, preventive, and alternative healing methods. The integration of these medical systems plays a crucial role in India’s healthcare policy, ensuring accessibility and affordability for all.
1. Allopathic System of Medicine
Key Features
- Scientific and Evidence-Based: Uses laboratory tests, clinical trials, and research-backed treatments.
- Symptom-Specific Treatment: Focuses on diagnosing diseases and providing targeted treatment.
- Pharmaceutical Drugs & Surgery: Relies on chemical drugs, antibiotics, and surgical interventions.
- Quick Relief: Immediate action against infections, trauma, and emergencies.
Major Components
- General Medicine: Internal medicine, treating common ailments.
- Surgery: Includes specialized fields like orthopedics, neurosurgery, cardiology.
- Pediatrics, Gynecology, and Oncology: Specialized branches for different patient demographics.
- Preventive Medicine: Vaccinations, public health campaigns, epidemiology.
Challenges
- Expensive Treatments: High costs for hospitalization, medicines, and surgeries.
- Overuse of Antibiotics: Leads to antibiotic resistance.
- Side Effects: Many drugs have adverse effects on organs and overall health.
- Unequal Access: Urban concentration of hospitals, while rural areas lack facilities.
Government Initiatives
- Ayushman Bharat: World’s largest health insurance scheme.
- Jan Aushadhi Yojana: Provides affordable generic medicines.
- National Health Mission (NHM): Strengthens public healthcare services.
- Universal Immunization Programme (UIP): Vaccination against life-threatening diseases.
2. Indian System of Medicine (AYUSH)
The Indian System of Medicine, under AYUSH, integrates traditional healing practices with modern healthcare.
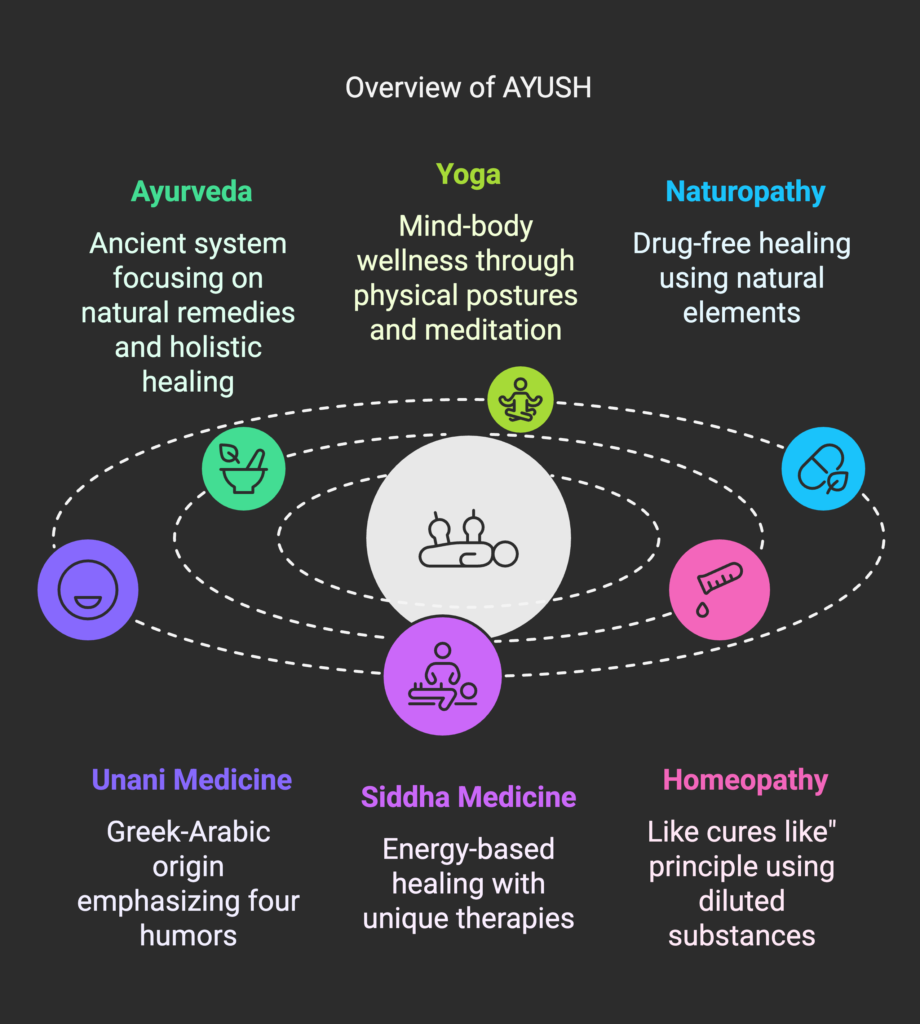
2.1 Ayurveda
- Ancient medical system (5000+ years old), based on natural remedies and holistic healing.
- Concept of Doshas (Vata, Pitta, Kapha) determines body constitution.
- Treatment Methods: Herbal medicines, Panchakarma therapy, dietary changes.
- Popular Ayurvedic Medicines: Ashwagandha (stress relief), Triphala (digestion), Brahmi (memory booster).
- Challenges: Standardization issues, slow acceptance in modern medicine, regulatory gaps.
Government Initiatives:
- National AYUSH Mission: Promotes research and integration into public health.
- All India Institute of Ayurveda (AIIA): Advanced research and development center.
- E-Aushadhi Portal: Online inventory management for AYUSH medicines.
2.2 Yoga
- Mind-Body Wellness: Incorporates physical postures (Asanas), breathing exercises (Pranayama), and meditation.
- Scientific Benefits: Enhances flexibility, reduces stress, improves cardiovascular health.
- Global Recognition: UN declared International Yoga Day (June 21).
- Integration in Healthcare: Used in lifestyle disease management (diabetes, hypertension).
Government Initiatives:
- Morarji Desai National Institute of Yoga (MDNIY): Promotes research and training.
- Common Yoga Protocol (CYP): Standardized yoga practice for mass adoption.
- Yoga Certification Board (YCB): Regulates yoga professionals.
2.3 Naturopathy
- Drug-Free Healing System: Uses natural elements like air, water, sunlight, diet, and exercise.
- Principles: Body’s self-healing capacity, prevention over cure, toxin removal.
- Therapies: Hydrotherapy, Mud therapy, Fasting therapy, Reflexology.
- Challenges: Lack of standardization, scientific validation, and integration with mainstream medicine.
Government Initiatives:
- National Institute of Naturopathy (NIN): Research and promotion.
- Naturopathy Wellness Centers: Established across India for holistic healthcare.
2.4 Unani Medicine
- Greek-Arabic origin, emphasizes four humors (Blood, Phlegm, Yellow Bile, Black Bile).
- Medicines: Herbal formulations, minerals, dietary therapy.
- Common Treatments: Skin diseases, digestive disorders, sexual health.
Government Support:
- Central Council for Research in Unani Medicine (CCRUM): Research and validation.
2.5 Siddha Medicine
- Ancient Tamil system, similar to Ayurveda, with energy-based healing.
- Medicines: Herbs, metals, minerals, animal products.
- Unique Therapies: Kaya Kalpa (rejuvenation), Varma (pressure points).
Government Support:
- National Institute of Siddha (NIS): Research and standardization.
2.6 Homeopathy
- “Like Cures Like” Principle: Uses highly diluted natural substances.
- Popular in India: Cost-effective, minimal side effects.
- Challenges: Scientific skepticism, placebo effect controversy.
Government Support:
- Central Council for Research in Homeopathy (CCRH): Standardization and research.
3. Comparative Analysis: Allopathy vs. AYUSH
| Feature | Allopathy | AYUSH (Ayurveda, Yoga, Unani, Siddha, Homeopathy) |
|---|---|---|
| Approach | Symptom-based | Holistic and preventive |
| Treatment | Drugs, surgery | Herbal, natural, and lifestyle-based |
| Side Effects | Possible adverse effects | Minimal side effects |
| Standardization | Well-regulated | Ongoing regulation efforts |
| Emergency Use | Effective | Limited |
| Scientific Validation | Strong evidence-based approach | Some systems lack rigorous scientific trials |
4. Committees & Reports on AYUSH
- National Health Policy (2017): Integration of AYUSH into primary healthcare.
- NITI Aayog Report on Traditional Medicine: Highlights the role of Ayurveda in preventive healthcare.
- WHO Traditional Medicine Strategy (2014-2023): Encourages global acceptance and integration of traditional medicine.
5. Current Affairs & Relevance
- COVID-19 & Immunity: Surge in Ayurveda and Homeopathy usage for immunity boosters.
- Global AYUSH Expansion: India signed agreements with the WHO Global Centre for Traditional Medicine.
- Telemedicine in AYUSH: Increasing use of digital platforms for remote consultation.
- AYUSH Startups: Growth of herbal medicine companies (Patanjali, Himalaya, Baidyanath).
Conclusion & Way Forward
Both Allopathy and AYUSH play vital roles in India’s healthcare system. While allopathy is essential for acute and emergency care, AYUSH offers sustainable, preventive, and holistic approaches to well-being. The future of healthcare lies in their integrated approach, ensuring accessible and affordable healthcare for all.
Way Forward
✔ Integrating AYUSH into Primary Healthcare: Standardized treatment protocols.
✔ Scientific Validation of AYUSH Medicines: Conducting large-scale clinical trials.
✔ Promoting Medical Tourism: Leveraging Ayurveda and Yoga.
✔ Public Awareness & Education: Encouraging people to adopt AYUSH for preventive care.
✔ Increased Government Investment in AYUSH Research: Strengthening R&D and production of herbal medicines.
NRHM, National HIV Programme, Tuberculosis Programme, and Preventive & Social Medicine (P&SM)
Introduction
Public health programs play a crucial role in controlling diseases, improving healthcare infrastructure, and promoting preventive measures. India has launched several initiatives, such as the National Rural Health Mission (NRHM), National HIV/AIDS Control Programme, Revised National Tuberculosis Control Programme (RNTCP), and Preventive & Social Medicine (P&SM), to address various public health challenges.
1. National Rural Health Mission (NRHM)
Introduction
Launched in 2005 under the National Health Mission (NHM), the NRHM focuses on improving rural healthcare services, especially for marginalized populations.
Objectives
- Strengthen healthcare delivery in rural areas.
- Reduce infant mortality rate (IMR) and maternal mortality rate (MMR).
- Increase institutional deliveries and access to skilled birth attendants.
- Improve primary healthcare infrastructure.
Key Features
- Accredited Social Health Activist (ASHA): Community-based health workers for awareness and maternal-child health support.
- Janani Suraksha Yojana (JSY): Incentives for institutional deliveries.
- National Mobile Medical Units: Provides doorstep healthcare services.
- Rogi Kalyan Samiti (RKS): Community involvement in hospital management.
- Strengthening of Sub-centers, Primary Health Centers (PHCs), and Community Health Centers (CHCs).
Achievements
- Increase in institutional deliveries from 47% (2005) to 83% (2021).
- Significant decline in IMR (30 per 1000 live births) and MMR (97 per 1 lakh live births).
- Strengthened rural healthcare infrastructure.
Challenges
- Shortage of doctors and specialists in rural areas.
- Inadequate funding in some states.
- Unequal access to healthcare in remote areas.
Government Initiatives
- Ayushman Bharat-Health and Wellness Centres (AB-HWCs): Strengthening primary healthcare.
- Pradhan Mantri Jan Arogya Yojana (PM-JAY): Free health insurance for the poor.
2. National HIV/AIDS Control Programme (NACP)
Introduction
India launched the National AIDS Control Programme (NACP) in 1992 to combat the HIV/AIDS epidemic. The current phase, NACP-V (2021-2026), focuses on prevention, treatment, and reducing stigma.
Objectives
- Reduce new HIV infections by 80% (baseline 2010).
- Increase Antiretroviral Therapy (ART) coverage.
- Strengthen HIV surveillance and awareness.
- Promote safe sex practices and harm reduction strategies.
Key Features
- Targeted Interventions (TI): Focused on high-risk groups (sex workers, IV drug users, MSM).
- HIV Testing & Counseling (HTC): Free and confidential HIV testing.
- Antiretroviral Therapy (ART): Free treatment under National AIDS Control Organisation (NACO).
- Prevention of Parent-to-Child Transmission (PPTCT).
- HIV/AIDS (Prevention & Control) Act, 2017: Prohibits discrimination against HIV-positive individuals.
Achievements
- New HIV infections reduced by 46% (2010-2020).
- ART coverage expanded, increasing life expectancy of HIV-positive individuals.
- Public awareness programs reduced stigma and increased voluntary testing.
Challenges
- High prevalence in certain states (Maharashtra, Andhra Pradesh, Karnataka, Tamil Nadu).
- Social stigma and discrimination.
- Funding gaps in prevention programs.
Government & Global Support
- National AIDS Control Organisation (NACO) under the Ministry of Health.
- Global Fund & UNAIDS collaborations.
- “95-95-95” Goal: By 2030, 95% of people should know their HIV status, 95% should be on ART, and 95% should have viral suppression.
3. Revised National Tuberculosis Control Programme (RNTCP)
Introduction
India has the highest TB burden globally. The RNTCP was launched in 1997, later rebranded as the National TB Elimination Programme (NTEP) in 2020.
Objectives
- Eliminate TB by 2025 (5 years ahead of the WHO goal of 2030).
- Provide free TB diagnosis and treatment.
- Ensure universal drug susceptibility testing.
- Strengthen TB surveillance and monitoring.
Key Features
- Directly Observed Treatment, Short-course (DOTS): Ensures adherence to TB treatment.
- Nikshay Poshan Yojana: ₹500/month financial support for TB patients.
- Free Drug-Resistant TB (DR-TB) Treatment: Special focus on Multidrug-Resistant TB (MDR-TB).
- Private Sector Engagement: Reporting of TB cases by private hospitals and doctors.
Achievements
- TB incidence reduced by 24% (2015-2022).
- Over 1.5 crore TB patients treated under the DOTS program.
- Introduction of newer TB drugs (Bedaquiline, Delamanid) for drug-resistant TB.
Challenges
- Rising Drug-Resistant TB (DR-TB) cases.
- Delayed detection in rural areas.
- Social stigma leads to underreporting.
- High burden among malnourished and HIV-infected populations.
Government Initiatives & International Collaborations
- TB Harega, Desh Jeetega: Awareness campaign.
- WHO End TB Strategy: Supports India’s goal of TB-free India by 2025.
- Stop TB Partnership: Global collaboration to fight TB.
4. Preventive and Social Medicine (P&SM)
Introduction
P&SM, also known as Community Medicine, focuses on preventive healthcare, epidemiology, and social determinants of health.
Objectives
- Prevent disease occurrence.
- Promote healthy lifestyles and nutrition.
- Conduct epidemiological research.
- Improve maternal and child health.
Key Aspects
- Epidemiology: Studies disease patterns and outbreaks.
- Vaccination Programs: Routine immunization, pulse polio campaign.
- Public Health Education: Awareness about hygiene, sanitation, nutrition.
- Environmental Health: Impact of pollution, water contamination, vector-borne diseases.
- Health Promotion: Lifestyle modification for diabetes, hypertension, obesity.
Major Programs Under P&SM
- Universal Immunization Programme (UIP): Vaccination against measles, polio, hepatitis B.
- Mission Indradhanush: Expanding immunization coverage.
- Swachh Bharat Abhiyan: Clean drinking water and sanitation.
- National Programme for Non-Communicable Diseases (NCDs): Addresses diabetes, hypertension, cancer.
Challenges
- Lack of preventive healthcare awareness.
- Inadequate healthcare workforce in public health.
- Need for better surveillance and data collection.
Conclusion & Way Forward
India has made significant strides in healthcare accessibility and disease control through programs like NRHM, NACP, NTEP, and P&SM. However, challenges like funding gaps, rural healthcare access, and disease burden persist.
Way Forward
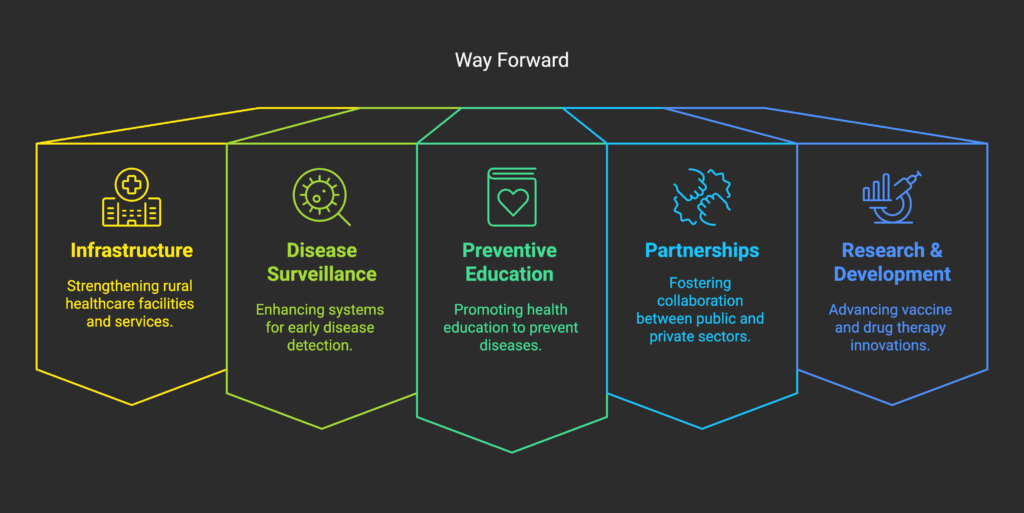
A multi-sectoral approach integrating preventive, curative, and rehabilitative healthcare is essential to achieve Universal Health Coverage (UHC) in India.
Diseases – Communicable Diseases, Epidemic Diseases, Endemic Diseases, and Vector-Borne Diseases
Introduction
Diseases can be classified based on their mode of transmission, spread, and geographical prevalence. Understanding different types of diseases—communicable, epidemic, endemic, and vector-borne—is crucial for public health planning and disease control strategies.
1. Communicable Diseases
Definition
Communicable diseases are caused by pathogens (bacteria, viruses, fungi, or parasites) and can be transmitted from one person to another through direct or indirect means.
Modes of Transmission
- Direct Contact: Physical touch, sexual contact (e.g., HIV, Syphilis).
- Airborne Transmission: Inhalation of droplets (e.g., Tuberculosis, COVID-19).
- Waterborne Transmission: Contaminated water (e.g., Cholera, Typhoid).
- Foodborne Transmission: Ingesting contaminated food (e.g., Hepatitis A).
- Vector-Borne Transmission: Through insects (e.g., Malaria, Dengue).
Examples of Communicable Diseases
| Disease | Causative Agent | Mode of Transmission | Prevention |
|---|---|---|---|
| Tuberculosis | Mycobacterium tuberculosis | Airborne | BCG Vaccine, Early Diagnosis |
| HIV/AIDS | Human Immunodeficiency Virus | Sexual, Bloodborne | Safe sex practices, ART therapy |
| Cholera | Vibrio cholerae | Contaminated Water | Safe drinking water, Sanitation |
| Influenza | Influenza virus | Airborne | Vaccination, Hygiene |
| Hepatitis B | Hepatitis B Virus | Bloodborne | Vaccination, Safe medical practices |
Prevention & Control
- Vaccination Programs (e.g., Universal Immunization Programme).
- Public Health Hygiene (sanitation, clean drinking water).
- Early Diagnosis & Treatment (screening and disease surveillance).
- Health Education & Awareness Campaigns.
2. Epidemic Diseases
Definition
An epidemic occurs when a disease spreads rapidly and affects a large number of people in a particular area or population within a short period.
Causes of Epidemics
- Poor sanitation and hygiene.
- Low immunity levels in a population.
- Increased human interaction and urbanization.
- Climate change affecting pathogen survival.
Examples of Epidemic Diseases in India
| Epidemic | Year | Cause | Impact |
|---|---|---|---|
| COVID-19 | 2020-2023 | SARS-CoV-2 virus | Global pandemic, lockdowns, economic crisis |
| Swine Flu (H1N1) | 2009 | H1N1 virus | Widespread infections, high fatality rate |
| Plague in Surat | 1994 | Yersinia pestis | Panic, migration, public health crisis |
| Japanese Encephalitis | 2017 | Flavivirus (mosquito-borne) | Affects brain, high mortality in children |
Government Responses to Epidemics
- Epidemic Diseases Act, 1897: Legal framework for epidemic control.
- National Centre for Disease Control (NCDC): Monitors and manages outbreaks.
- Integrated Disease Surveillance Programme (IDSP): Early warning system.
- COVID-19 Management Strategies: Lockdowns, vaccination drives, genome sequencing.
Prevention & Control Measures
- Rapid Response Teams (RRTs) to contain outbreaks.
- Public Awareness Campaigns (e.g., Swachh Bharat Abhiyan for hygiene).
- Quarantine & Isolation Protocols during infectious disease outbreaks.
- Research & Development for vaccines and treatments.
3. Endemic Diseases
Definition
An endemic disease is a disease that is constantly present in a particular region or population but remains relatively stable in terms of case numbers.
Causes of Endemic Diseases
- Climatic and geographical conditions (e.g., Malaria in tropical regions).
- Lack of healthcare access in certain areas.
- Socioeconomic conditions (e.g., poor nutrition, overcrowding).
Examples of Endemic Diseases in India
| Disease | Region Affected | Cause | Control Measures |
|---|---|---|---|
| Malaria | Northeast, Odisha, Chhattisgarh | Plasmodium parasite (Mosquito-borne) | Insecticide-treated bed nets, Anti-malarial drugs |
| Tuberculosis | Nationwide | Mycobacterium tuberculosis | DOTS therapy, BCG vaccination |
| Kala Azar (Visceral Leishmaniasis) | Bihar, Jharkhand, West Bengal | Leishmania parasite (Sandfly vector) | Vector control, Amphotericin B treatment |
| Dengue | Urban and semi-urban areas | Aedes mosquito | Mosquito control measures, Dengue vaccine trials |
Government Initiatives
- National Vector-Borne Disease Control Programme (NVBDCP): Controls endemic vector-borne diseases.
- Revised National Tuberculosis Control Programme (RNTCP): Now known as National TB Elimination Programme (NTEP).
- National Malaria Eradication Programme (NMEP): Focus on Malaria-free India by 2030.
4. Vector-Borne Diseases
Definition
Vector-borne diseases are transmitted through insects and other arthropods, such as mosquitoes, ticks, and fleas.
Major Vectors & Associated Diseases
| Vector | Disease | Causative Agent | Affected Areas |
|---|---|---|---|
| Mosquito (Aedes) | Dengue, Chikungunya | Virus | Urban & semi-urban India |
| Mosquito (Anopheles) | Malaria | Plasmodium parasite | Northeast, Odisha, Jharkhand |
| Mosquito (Culex) | Japanese Encephalitis | Flavivirus | Bihar, Uttar Pradesh |
| Sandfly | Kala Azar | Leishmania parasite | Bihar, Jharkhand, West Bengal |
| Tick | Lyme Disease | Borrelia bacteria | Hills & forest regions |
Prevention & Control Measures
- Elimination of Breeding Grounds: Avoid water stagnation, use larvicides.
- Personal Protection Measures: Mosquito nets, insect repellents, full-sleeve clothing.
- Vaccination & Prophylaxis: Dengue vaccine development, Malaria prophylaxis.
- Vector Control Programs: Government fumigation and awareness campaigns.
Government Initiatives for Vector-Borne Disease Control
- National Vector Borne Disease Control Programme (NVBDCP).
- Malaria Elimination Strategy (2016-2030): Reduce cases to zero by 2030.
- Dengue & Chikungunya Control Programme: Public health education and surveillance.
Conclusion & Way Forward
Diseases, whether communicable, epidemic, endemic, or vector-borne, pose significant public health challenges in India. Effective disease surveillance, vaccination, healthcare infrastructure, and community participation are essential to prevent and control their spread.
Way Forward
✔ Strengthening Primary Healthcare: Accessible healthcare in rural and tribal areas.
✔ Early Diagnosis & Rapid Response: Improved disease surveillance mechanisms.
✔ Investments in Research & Vaccination: Focus on emerging infectious diseases.
✔ Public Awareness & Behavioral Change: Hygiene, nutrition, sanitation campaigns.
✔ Global Collaboration: WHO, GAVI, and international partnerships for disease control.
By integrating modern medicine with public health strategies, India can achieve effective disease control, lower mortality rates, and improved public health outcomes.
Vaccines, Introduction to Immunity, and Production of DPT, Rabies, and Hepatitis Vaccines
Introduction
Vaccines are biological preparations that provide immunity against specific infectious diseases. They stimulate the body’s immune system to recognize and fight pathogens, reducing the risk of infections and associated complications. Vaccination has played a pivotal role in global public health, helping to control and eradicate diseases such as smallpox and polio.
1. Introduction to Immunity
Definition
Immunity is the body’s ability to resist infections through the activation of immune responses. It can be natural (innate) or acquired (adaptive).
Types of Immunity
| Type | Description | Example |
|---|---|---|
| Innate Immunity | Natural defense present from birth; non-specific response. | Skin barrier, phagocytosis |
| Acquired Immunity | Develops after exposure to pathogens or vaccines. | Post-infection immunity, vaccination |
| Active Immunity | Body produces its own antibodies. | Vaccination, recovery from infection |
| Passive Immunity | Antibodies transferred from another source. | Maternal antibodies in newborns, antibody injections |
Immune Response Process
- Recognition: White blood cells identify antigens (foreign substances).
- Activation: Immune cells (B-cells, T-cells) respond by producing antibodies or killing infected cells.
- Memory Formation: The immune system “remembers” the pathogen for faster response in future infections.
Role of Vaccines in Immunity
- Mimic natural infections to stimulate an immune response without causing disease.
- Memory cells ensure long-term protection.
- Herd immunity helps protect those who cannot be vaccinated (e.g., immunocompromised individuals).
2. Types of Vaccines
| Type | Description | Example |
|---|---|---|
| Live Attenuated Vaccines | Contain weakened pathogens that do not cause severe disease. | MMR (Measles, Mumps, Rubella), BCG, Oral Polio Vaccine |
| Inactivated (Killed) Vaccines | Contain killed pathogens, requiring booster doses. | Hepatitis A, Rabies |
| Toxoid Vaccines | Contain inactivated toxins produced by bacteria. | Diphtheria, Tetanus (DPT) |
| Subunit & Conjugate Vaccines | Use parts of pathogens (proteins or sugars) to trigger immunity. | Hepatitis B, HPV |
| mRNA Vaccines | Use genetic instructions to produce viral proteins. | COVID-19 (Pfizer, Moderna) |
3. Production of DPT Vaccine
Introduction
The DPT vaccine provides immunity against Diphtheria, Pertussis (Whooping Cough), and Tetanus. It is a combination vaccine that protects against three serious bacterial infections.
Production Process
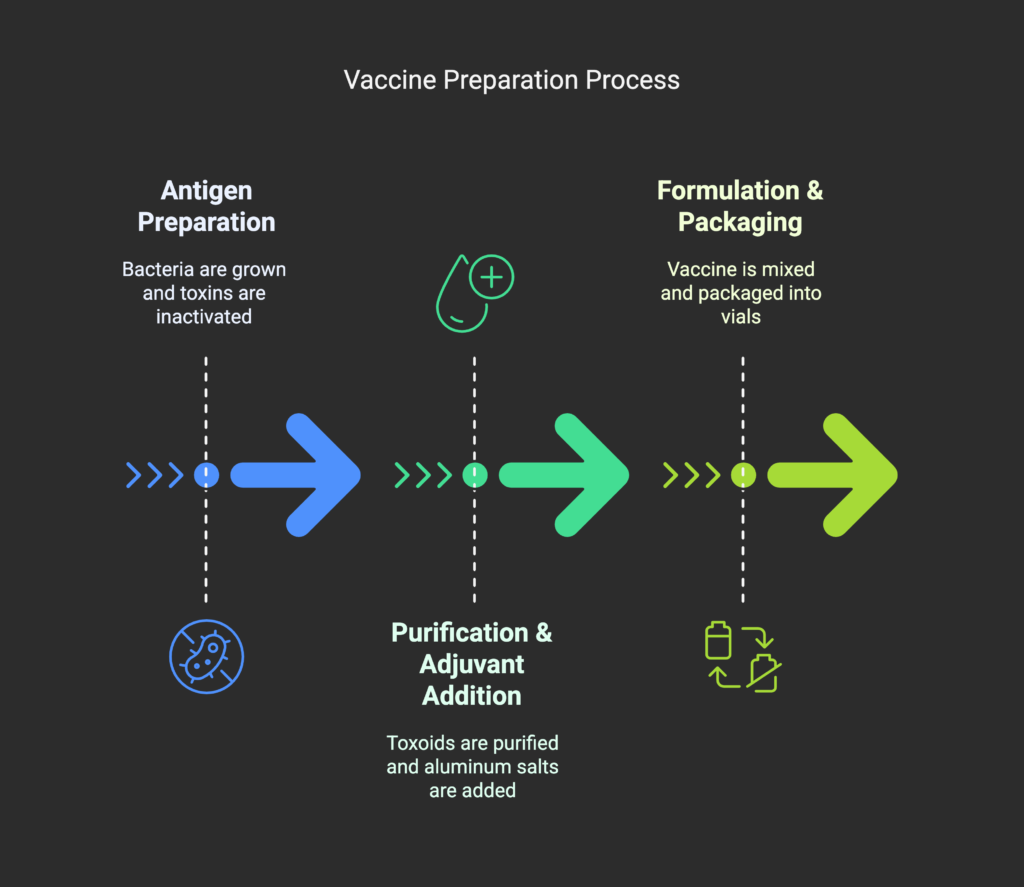
- Antigen Preparation
- Diphtheria & Tetanus Toxoid: The bacteria Corynebacterium diphtheriae and Clostridium tetani are grown in a controlled environment, and their toxins are inactivated using formaldehyde.
- Pertussis Component: The Bordetella pertussis bacterium is inactivated (whole-cell or acellular).
- Purification & Adjuvant Addition
- The toxoids and inactivated bacteria are purified.
- Aluminum salts (adjuvants) are added to enhance the immune response.
- Formulation & Packaging
- The vaccine is mixed in precise proportions and packaged into vials or pre-filled syringes.
DPT Vaccination Schedule
- Given at: 6, 10, and 14 weeks of age, with booster doses at 16-24 months and 5-6 years.
- Side Effects: Mild fever, swelling at the injection site, irritability.
Government Initiative
- Universal Immunization Programme (UIP) provides free DPT vaccination to all infants in India.
4. Production of Rabies Vaccine
Introduction
The rabies vaccine is essential for preventing rabies, a deadly viral infection transmitted through animal bites. It is administered as post-exposure prophylaxis (PEP) and pre-exposure prophylaxis (PrEP) for high-risk individuals.
Types of Rabies Vaccines
- Cell Culture-Based Vaccines (Modern vaccines): Vero cell rabies vaccine (VCRV), Human diploid cell vaccine (HDCV).
- Nerve Tissue-Based Vaccines (Outdated, phased out due to side effects).
Production Process
- Virus Cultivation
- The rabies virus is grown in cell cultures (Vero cells or human diploid cells).
- Inactivation
- The virus is killed using β-propiolactone, ensuring it cannot cause disease but can trigger an immune response.
- Purification & Stabilization
- The vaccine is purified and stabilized with preservatives (e.g., human albumin).
- Formulation & Packaging
- The vaccine is formulated into single-dose or multi-dose vials.
Administration & Dosage
- Post-exposure prophylaxis (PEP): Given on days 0, 3, 7, 14, 28 after exposure.
- Pre-exposure prophylaxis (PrEP): For veterinarians, animal handlers, and travelers to rabies-endemic areas.
Government Initiatives
- National Rabies Control Programme (NRCP) aims to eliminate rabies by 2030 through mass dog vaccination and awareness.
5. Production of Hepatitis Vaccines
Introduction
Hepatitis is a viral infection affecting the liver, caused by Hepatitis A, B, C, D, and E viruses. Vaccination is available for Hepatitis A and B.
Hepatitis B Vaccine Production
- Gene Insertion in Yeast Cells
- The Hepatitis B surface antigen (HBsAg) gene is inserted into Saccharomyces cerevisiae (yeast cells) using recombinant DNA technology.
- Protein Production & Extraction
- The yeast cells produce the antigen, which is then extracted and purified.
- Formulation with Adjuvants
- The purified antigen is mixed with Aluminum hydroxide (adjuvant) to boost immunity.
- Packaging & Storage
- The vaccine is packed into sterile vials and stored at 2-8°C.
Hepatitis A Vaccine Production
- Produced using inactivated Hepatitis A virus grown in cell cultures.
- The virus is killed using formaldehyde and formulated for injection.
Vaccination Schedule
- Hepatitis A Vaccine: Given at 1 year of age (single or two-dose schedule).
- Hepatitis B Vaccine: Given at birth, 6 weeks, 10 weeks, and 14 weeks, with a booster at 6 months.
Government Initiatives
- National Viral Hepatitis Control Programme (NVHCP) aims to eliminate Hepatitis B & C by 2030.
Conclusion & Way Forward
Vaccination remains one of the most effective public health measures in combating infectious diseases. DPT, Rabies, and Hepatitis vaccines play a crucial role in reducing morbidity and mortality worldwide.
Way Forward
✔ Increase vaccine coverage through awareness and rural outreach programs.
✔ Research & Development in vaccine technology (e.g., mRNA vaccines for more diseases).
✔ Strengthening the cold chain system for vaccine storage and distribution.
✔ Enhancing global collaborations for disease eradication initiatives.
With continuous advancements in immunization programs and vaccine technology, a disease-free future is within reach.
Application of Immunological Methods in Diagnosis
Introduction
Immunological methods play a crucial role in disease diagnosis, surveillance, and treatment monitoring by detecting antigens, antibodies, and immune responses. These methods are widely used in medical diagnostics, forensic science, biotechnology, and vaccine development. Immunological techniques provide rapid, sensitive, and specific detection of infectious and non-infectious diseases.
1. Principles of Immunological Diagnostic Methods
Key Components
- Antigen (Ag): A foreign substance (pathogen, toxin, or molecule) that triggers an immune response.
- Antibody (Ab): A protein produced by the immune system to neutralize antigens.
- Immune Complex Formation: Binding of antibodies to antigens helps in disease detection.
Types of Immunological Reactions in Diagnosis
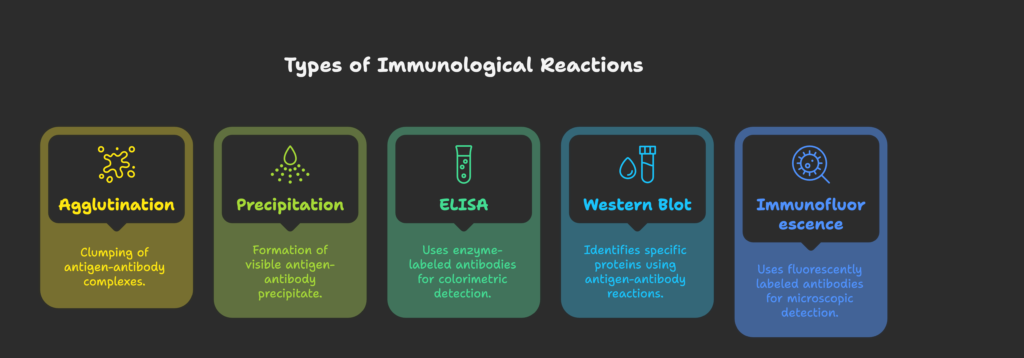
2. Immunological Methods in Disease Diagnosis
2.1 Serological Tests
Definition: Detect antibodies or antigens in blood serum to diagnose infections.
Applications
| Method | Disease Diagnosed | Principle |
|---|---|---|
| Widal Test | Typhoid | Agglutination of Salmonella antigens with patient serum |
| Weil-Felix Test | Rickettsial infections | Agglutination test with Proteus antigens |
| VDRL Test | Syphilis | Detects antibodies against Treponema pallidum |
| Dengue IgM/IgG Test | Dengue Fever | Detects virus-specific antibodies |
| HIV Rapid Test | HIV/AIDS | Antibody-antigen detection in blood |
2.2 Enzyme-Linked Immunosorbent Assay (ELISA)
Principle: Uses enzyme-labeled antibodies to detect antigens or antibodies in a sample.
Types:
- Direct ELISA: Detects antigen using a single enzyme-labeled antibody.
- Indirect ELISA: Detects antibody using an additional secondary antibody.
- Sandwich ELISA: Uses two antibodies to capture and detect antigen.
Applications:
✔ HIV Testing (Detects p24 antigen).
✔ Hepatitis B & C Detection.
✔ COVID-19 Antibody Testing.
✔ Hormone Level Testing (e.g., Pregnancy tests for hCG hormone).
2.3 Western Blot
Principle: Identifies specific proteins by gel electrophoresis, transfer to a membrane, and antigen-antibody reaction.
Applications:
✔ Confirmatory test for HIV.
✔ Detects Lyme disease and Hepatitis B proteins.
✔ Used in protein-based forensic investigations.
2.4 Immunofluorescence (IF) and Flow Cytometry
Principle: Uses fluorescently labeled antibodies to detect antigens in tissues or cells.
Types of Immunofluorescence
| Method | Application |
|---|---|
| Direct Immunofluorescence (DIF) | Autoimmune disease diagnosis (Pemphigus, Lupus) |
| Indirect Immunofluorescence (IIF) | Viral infections (Herpes, Rabies) |
| Flow Cytometry | Cancer (Leukemia, Lymphoma) & Immune profiling |
2.5 Rapid Immunochromatographic Tests
Principle: Lateral flow assays (LFA) use antigen-antibody interactions on a test strip for quick disease detection.
Examples:
✔ Pregnancy Test (hCG detection).
✔ COVID-19 Rapid Antigen Test.
✔ Malaria Rapid Diagnostic Test.
✔ Hepatitis B Surface Antigen (HBsAg) Test.
3. Immunological Methods in Autoimmune & Cancer Diagnosis
Autoimmune Disease Diagnosis
✔ Anti-Nuclear Antibody (ANA) Test → Detects Lupus & Rheumatoid Arthritis.
✔ Rheumatoid Factor (RF) Test → Diagnoses Rheumatoid Arthritis.
✔ Thyroid Peroxidase Antibody Test → Diagnoses Hashimoto’s Thyroiditis.
Cancer Diagnosis Using Immunology
✔ Tumor Marker Detection (e.g., PSA for Prostate Cancer, CA-125 for Ovarian Cancer).
✔ Immunohistochemistry (IHC) → Detects cancer biomarkers in tissues.
✔ Monoclonal Antibody Therapy → Used for targeted cancer treatment (e.g., Rituximab for Lymphoma).
4. Advances in Immunodiagnostics
4.1 Monoclonal Antibody-Based Diagnostics
- Used in COVID-19 testing kits (e.g., SARS-CoV-2 antigen test).
- Application in precision medicine for cancer therapy.
4.2 Biosensors in Immunology
- Uses nanotechnology and microfluidics for ultra-sensitive diagnostics.
- Smartphone-based ELISA kits improve accessibility.
4.3 CRISPR-Based Immunodiagnostics
- SHERLOCK and DETECTR techniques use gene-editing technology for rapid viral detection.
- Future applications: Point-of-care genetic disease diagnostics.
5. Government Initiatives for Immunodiagnostic Advancements
✔ National Immunization Programme (UIP) → Strengthens vaccine-based immunity and diagnostic research.
✔ National Centre for Disease Control (NCDC) → Oversees immunological disease surveillance.
✔ Indian Council of Medical Research (ICMR) → Develops new immunodiagnostic techniques.
✔ WHO Collaboration on Global Disease Monitoring → Strengthens immunology-based global health surveillance.
Conclusion & Way Forward
Immunological methods have revolutionized medical diagnostics, making disease detection faster, more accurate, and cost-effective. The future of diagnostics lies in molecular immunology, AI-driven diagnostics, and personalized medicine.
Way Forward
✔ Strengthening Immunodiagnostic Infrastructure in rural and underserved areas.
✔ Investment in AI & Machine Learning for rapid immunological test analysis.
✔ Research on Novel Antibody-Based Therapeutics for emerging infectious diseases.
✔ Integration of Digital Health Technologies with immunodiagnostic data for real-time disease tracking.
By leveraging advanced immunological techniques, India can enhance its healthcare system, improve disease control, and strengthen epidemic preparedness.
Health Awareness Programme
Introduction
Health awareness programs play a crucial role in educating the public about diseases, preventive healthcare, hygiene, nutrition, and lifestyle choices. These programs aim to reduce the burden of communicable and non-communicable diseases (NCDs) by promoting early detection, immunization, and health-seeking behavior.
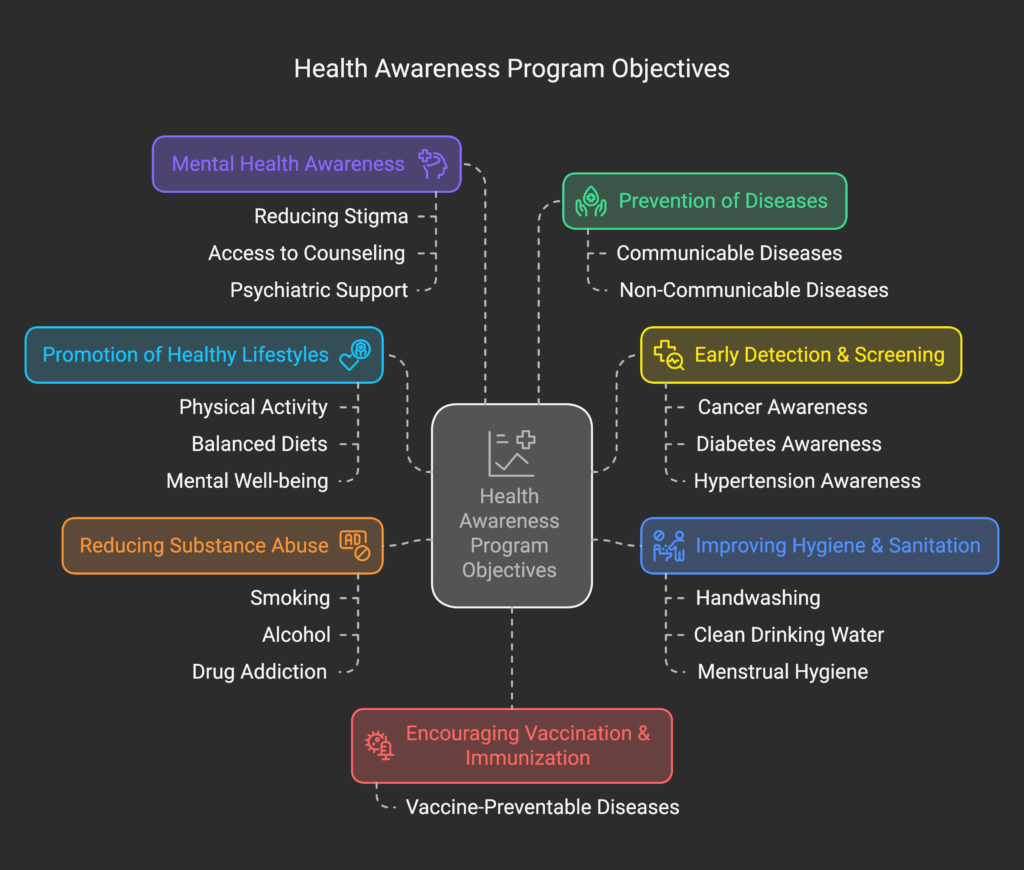
1. Objectives of Health Awareness Programmes
2. Major Health Awareness Programmes in India
2.1 Communicable Disease Awareness Programmes
| Programme | Objective | Key Features |
|---|---|---|
| National AIDS Control Programme (NACP) | HIV/AIDS Awareness | Free testing & ART therapy, Safe sex promotion |
| National Tuberculosis Elimination Programme (NTEP) | TB Awareness | Early TB detection, DOTS therapy, free diagnosis |
| National Vector Borne Disease Control Programme (NVBDCP) | Malaria, Dengue, Chikungunya Control | Mosquito control, awareness on bed nets, anti-larval measures |
| Pulse Polio Programme | Polio Eradication | Oral polio vaccine (OPV), mass immunization drives |
2.2 Non-Communicable Disease (NCD) Awareness Programmes
| Programme | Focus Area | Awareness Strategies |
|---|---|---|
| National Programme for Prevention & Control of Cancer, Diabetes, Cardiovascular Diseases & Stroke (NPCDCS) | NCD Awareness | Screening camps, yoga, lifestyle modifications |
| Fit India Movement | Physical Fitness | Awareness on exercise, diet, obesity prevention |
| National Tobacco Control Programme (NTCP) | Tobacco Awareness | Anti-smoking campaigns, graphic warning labels on cigarettes |
| Mental Health Awareness Programme | Psychological Health | Suicide prevention, stress management, depression counseling |
2.3 Maternal & Child Health Awareness Programmes
| Programme | Objective | Impact |
|---|---|---|
| Janani Suraksha Yojana (JSY) | Safe Motherhood | Promotes institutional deliveries |
| Poshan Abhiyan | Nutrition Awareness | Prevents malnutrition, promotes breastfeeding |
| Rashtriya Kishor Swasthya Karyakram (RKSK) | Adolescent Health | Educates on reproductive health, menstrual hygiene |
2.4 Hygiene & Sanitation Awareness Programmes
| Programme | Focus Area | Key Activities |
|---|---|---|
| Swachh Bharat Abhiyan | Cleanliness & Hygiene | Sanitation drives, toilet construction |
| National Deworming Programme | Worm Infestation | School-based deworming campaigns |
| Hand Hygiene Programme | Handwashing Awareness | Educating school children & healthcare workers |
2.5 Immunization Awareness Programmes
| Programme | Vaccine Covered | Target Group |
|---|---|---|
| Universal Immunization Programme (UIP) | Polio, Measles, Hepatitis B | Infants & Pregnant Women |
| Mission Indradhanush | Expands vaccine coverage | Unvaccinated children |
| COVID-19 Vaccination Drive | COVID-19 | Mass immunization campaigns |
3. Methods Used in Health Awareness Programmes
✔ Mass Media Campaigns: TV, radio, social media (e.g., Pulse Polio ads).
✔ Community Health Workers (ASHA, ANMs): Conduct door-to-door awareness.
✔ Health Camps & Free Screening: Early diagnosis for diabetes, TB, HIV.
✔ School & Workplace Health Programs: Educating students and employees on health.
✔ Collaborations with NGOs & Private Sector: Public-private partnerships for outreach.
4. Impact & Success Stories of Health Awareness Programmes
✔ Polio-Free India (2014): Due to aggressive Pulse Polio Programme.
✔ Decline in Maternal Mortality Rate (MMR): Due to Janani Suraksha Yojana.
✔ Tobacco Consumption Reduction: Due to anti-smoking campaigns under NTCP.
✔ COVID-19 Vaccination Achievement: Over 2 billion doses administered in India.
5. Challenges in Health Awareness Initiatives
❌ Lack of Awareness in Rural Areas: Low literacy affects program reach.
❌ Misinformation & Vaccine Hesitancy: Myths about vaccines and diseases.
❌ Funding Constraints: Limited budgets for nationwide campaigns.
❌ Behavioral Resistance: Difficulty in changing health habits (e.g., tobacco cessation).
❌ Logistics & Infrastructure: Shortage of healthcare personnel in remote areas.
6. Future Strategies & Way Forward
✔ Digital Health & Telemedicine: Expanding e-health awareness campaigns.
✔ Strengthening School Health Programs: Including health education in curriculum.
✔ Using AI & Big Data: Predictive analytics for disease outbreaks.
✔ Public-Private Partnerships: Engaging corporate social responsibility (CSR) in health programs.
✔ Localized & Vernacular Campaigns: Spreading awareness in regional languages.
Conclusion
Health awareness programs empower communities with knowledge to make informed health decisions. Strengthening awareness through innovative methods can significantly improve India’s public health outcomes and disease prevention. With policy support, community participation, and technological advancements, these programs can drive India towards “Health for All.”
